Normal hypnogram in a young adult. Wake (W), REM sleep (R), Light sleep stages (N1 and N2), and Deep sleep or slow wave sleep (N3) are plotted on the y axis. Time in hours is on the x axis. This graph was part of Dr. Barratt’s publication that was awarded the Editor’s Choice Special Distinction as an Exemplary Resource from the Association American of Medical College’s MedEdPORTAL. Citation—Barratt DM, Mader EC, Gutierrez A, and Oliva AA. EEG and Sleep Team-Based Learning. MedEdPORTAL Publications; https://www.mededportal.org
Wake, N1, and N2 sleep in a young adult. During normal healthy sleep, a young adult passes quickly from Wake through N1 and N2 sleep.
N1 and N2 are stages of light sleep.
Brain activity begins to slow and the body starts to relax; however, people are easily awakened from light sleep.
Periodic limb movements may occur during light sleep.
N3, or deep, slow wave sleep in a young adult. After brief periods of N1 and N2 sleep, a long period of N3 or slow wave sleep occurs.
Brain activity slows, the body relaxes, and there is a normal drop in blood pressure.
It is more difficult to awaken someone from deep or slow wave sleep.
Deep or slow wave sleep can be associated with confusional arousals, sleep-walking, and night terrors.
REM (rapid eye movement) sleep in a young adult. Ninety minutes after falling asleep, the first REM period occurs.
The mind and body are very active during REM sleep, and people can easily awaken. Upon awakening, they can remember their dreams.
During normal REM sleep, muscles (except the muscles controlling the eye movements and the diaphragm) are paralyzed to prevent one from acting out dreams.
In rare cases, a person is NOT paralyzed during REM sleep and enacts their dreams. This is known as REM Sleep Behavior Disorder.
Because of muscle paralysis, snoring and obstructive sleep apnea can become much worse during REM sleep.
Overall, young adults spend about 20% of their total sleep time in REM sleep.
The cycle repeats.
The cycle repeats itself approximately 5 times, with each period of deep, slow wave sleep becoming shorter and each period of REM sleep becoming longer.
Hypnogram in an older adult. Wake (W), REM sleep (R), Light sleep stages (N1 and N2), and Deep sleep or slow wave sleep (N3) are plotted on the y axis. Time in hours is on the x axis. This graph was part of Dr. Barratt’s publication that was awarded the Editor’s Choice Special Distinction as an Exemplary Resource from the Association American of Medical College’s MedEdPORTAL. Citation—Barratt DM, Mader EC, Gutierrez A, and Oliva AA. EEG and Sleep Team-Based Learning. MedEdPORTAL Publications; https://www.mededportal.org
Sleep Health and Sleep Disorders
As a board-certified sleep medicine physician, Dr. Barratt specializes in the promotion of healthy sleep and the treatment of sleep disorders. She treats insomnia, sleep apnea, narcolepsy, restless legs syndrome, and REM behavior disorder.
Question: Is sleep important?
Answer: Sleep is essential.
Lack of healthy sleep results in the following:
Brain fog
Poor memory consolidation
Impaired concentration
Processes that occur during normal sleep:
Encoding of memories for long-term storage
Clearance of the amyloid and tau proteins associated with Alzheimer's Disease
Question: What are the stages of sleep in a young adult, and how does that change as a person grows older?
Wake, N1, and N2 Sleep in older adults. An older adult may require more time to fall asleep and transition into N1 and N2 sleep.
The characteristics of N1 and N2, or light sleep, are the same, regardless of age.
Brain activity begins to slow and the body starts to relax; however, people are easily awakened from light sleep.
Older adults spend more time in light sleep and experience more frequent awakenings.
N3, or deep, slow wave sleep in older adults. Although the characteristics of slow wave sleep are the same regardless of age, older adults have a more difficult time achieving slow wave sleep.
Brain waves slow, the body relaxes, and there is a normal drop in blood pressure.
It is more difficult to awaken someone from deep or slow wave.
Deep or slow wave sleep can be associated with confusional arousals, sleep-walking, and night terrors.
REM (rapid eye movement) sleep in older adults. The characteristics of REM sleep are the same, regardless of age.
The mind and body are very active during REM sleep, and people can easily awaken. Upon awakening, they can remember their dreams.
During normal REM sleep, muscles (except the muscles controlling the eyes and the diaphragm) are paralyzed to prevent one from acting out dreams.
In rare cases, a person is not paralyzed during REM sleep and enacts dreams. This is known as REM Sleep Behavior Disorder.
Although the sleep cycles are less predictable, older adults spend approximately 20% of their total sleep time in REM sleep.
The cycle repeats.
As in young adults, the cycle repeats itself. However, sleep is more fragmented and less slow wave sleep occurs.
Question: If sleep changes as adults grow older, how does one know if there is a problem?
Answer: Older adults should understand that they may not sleep as soundly as they did when they were 20 years old. However, if they are experiencing severe insomnia or significant daytime sleepiness, there may be a problem. Take the Epworth Sleepiness Scale and call 561-300-4178 to schedule an appointment with Dr. Barratt.
Question: How common is obstructive sleep apnea, and why is it hazardous to one’s health?
Answer: An estimated 425 million people worldwide have obstructive sleep apnea.
During normal sleep, muscles of the tongue and throat relax. During REM sleep, muscles become paralyzed.
The relaxation and/or paralysis can cause the airway to collapse and breathing either stops (apnea) or slows (hypopnea).
Apneas and hypopneas can result in oxygen desaturations, awakenings, and even irregular heart rhythms, such as atrial fibrillation.
This disrupts the normal dip in blood pressure that should occur during sleep.
Heart rate increases, as does the heart’s demand for oxygen.
The above contribute to hypertension, enlargement of the heart, and atherosclerosis.
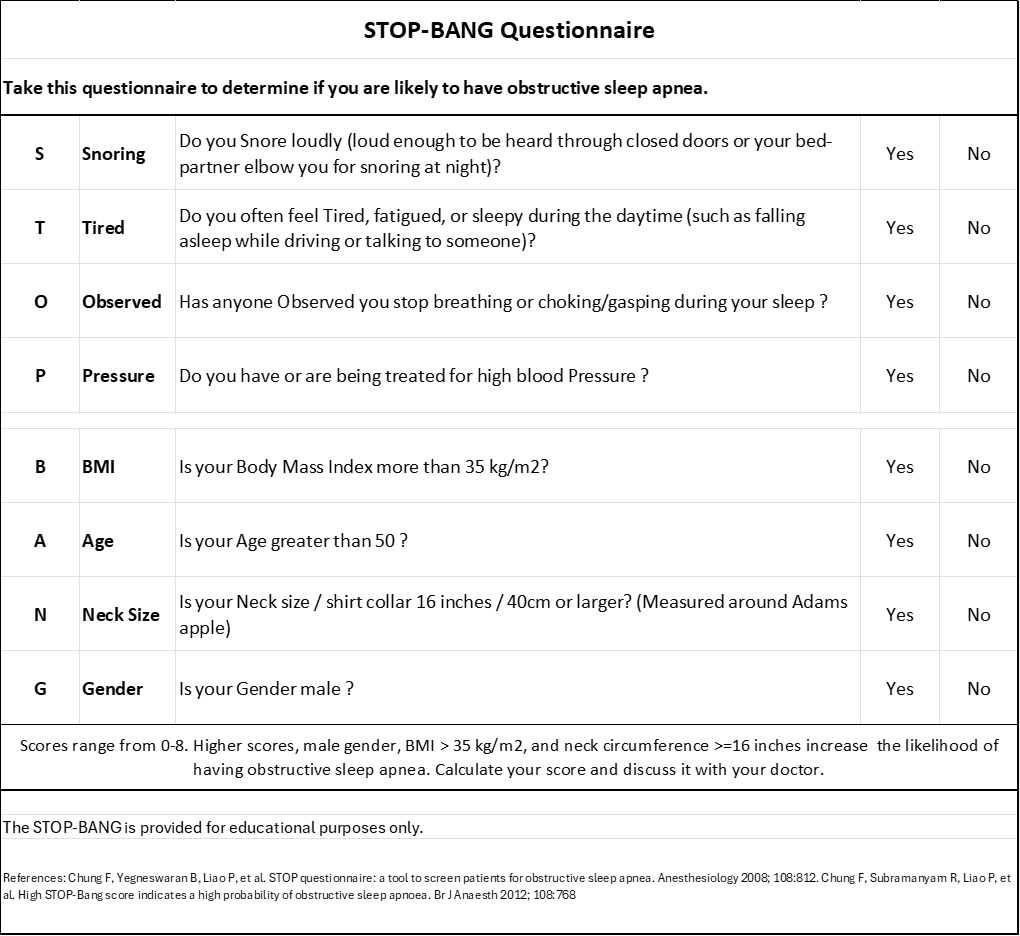
Question: How would a person know if he or she has obstructive sleep apnea?
Answer: Obstructive sleep apnea is suspected when the bed partner can hear the person snoring, choking, or gasping. There is a screening tool called the STOP BANG Questionnaire. A higher score makes it more likely that a person has obstructive sleep apnea.
Call 561-300-4178 to schedule an appointment with Dr. Barratt.
Question: Do women experience obstructive sleep apnea?
Answer: Women of all ages can experience obstructive sleep apnea. However, obstructive sleep apnea often presents differently in women. Women are more likely to develop obstructive sleep apnea after menopause. Additionally, they are less likely to report snoring and witnessed apneas and more likely to present with insomnia, fatigue, and daytime sleepiness.
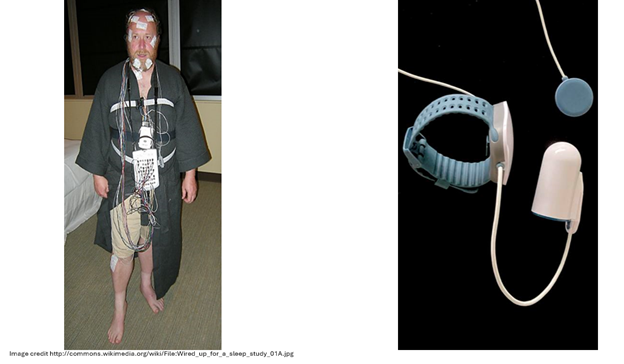
Pictured above is a patient undergoing an in-lab polysomnogram (overnight sleep study) and a home sleep test. The technology has improved a great deal over the last 20 years. Many patients would qualify for a home sleep test.
Question: How is the diagnosis of obstructive sleep apnea confirmed?
Answer: An overnight sleep study is required to confirm the diagnosis of obstructive sleep apnea.
Most patients would qualify for a home sleep apnea test.
The technology of home sleep testing has improved tremendously over the last 20 years.
Using a wristwatch, finger probe, and chest lead, one can record the following:
Light sleep
Deep sleep
REM sleep
Apnea hypopnea index
Oxygen saturations
Body position
Cardiac monitoring
Mechanisms of upper airway occlusion in Obstructive Sleep Apnea. Left: normal muscle tone prevents collapse of the upper airway. Middle: relaxation during sleep results in collapse of the airway and obstruction. Right: continuous positive airway pressure (CPAP) provides a pneumatic splint, keeping the upper airway open. (This image was part of Dr. Barratt’s publication that was awarded the Editor’s Choice Special Distinction as an Exemplary Resource from the Association American of Medical College’s MedEdPORTAL. Citation—Barratt DM, Mader EC, Gutierrez A, and Oliva AA. EEG and Sleep Team-Based Learning. MedEdPORTAL Publications; https://www.mededportal.org)
Question: What is the treatment for obstructive sleep apnea?
Answer: The good news is there are options.
CPAP, or continuous positive airway pressure is the most commonly prescribed treatment.
o CPAP is the best choice for severe obstructive sleep apnea.
o Patients, with the help of a respiratory therapist, select a mask, which fits over the nose or nose and mouth.
o The machine provides pressure, which prevents collapse of the airway.
o In addition to providing treatment, the machine monitors the number of hours the patient used the machine and the number of apneas that occurred overnight.
o Technology has improved and many patients tolerate CPAP very well.
o If you tried it in the past, and it did not work out for you, it may be worth another attempt.
Mandibular advancement devices are options for patients unwilling or unable to use CPAP.
o A dentist with specialized training in sleep medicine makes an oral appliance that brings the jaw forward.
o The advancement of the mandible results in opening of the airway.
Weight loss
o Weight loss is a conservative therapy that may result resolution of obstructive sleep apnea
o Your doctor can advise you on the different treatment options for weight loss.
Sleep position device
o Some patients only experience apneas while sleeping on their backs.
o An inexpensive sleep position device can prevent back sleeping and eliminate the need for more expensive and cumbersome treatments.
Speech pathologist for tongue exercises
o A speech pathologist can teach patients tongue strengthening exercises that will reduce snoring and apneas.
Daytime tongue stimulator for tongue strengthening
o An FDA-authorized device used during the daytime can strengthen the muscles of the tongue.
o This device can treat snoring or mild sleep apnea
Question: How do symptoms of menopause (or perimenopause) affect sleep in women?
Answer: The transition through menopause is different in every woman. Regarding sleep, some women experience hot flashes and night sweats that interfere with their ability to fall asleep and stay asleep. This can be a significant quality of life issue.
· Hormone replacement therapy may be appropriate for women experiencing night sweats and disturbed sleep.
· This is especially true if women are less than 60 years of age and < 10 years from the onset of menopause.
· Other options exist for women at high risk of blood clots, or those with heart disease, endometrial cancer, or breast cancer.
· With appropriate treatment, some women experience complete relief from symptoms of hot flashes, night sweats, and the accompanying sleep disruption.